Total Joint Arthroplasty: An Intensive Lab Course to Improve Functional Outcomes
Total joint arthroplasty is the most common surgical procedure performed in the U.S. and will continue to climb rapidly. However, as surgical advances and prosthetic implants improve rapidly, the therapeutic process and protocols used with this population have remained stagnant. In an attempt to improve outcomes while reducing length of stay and therapy visits, clinicians have over utilized rigid protocols while neglecting proprioception and function yielding a reduction in long term outcomes. Today’s clinician must possess a stronger understanding of the techniques used by surgeons, the prosthetics commonly (and uncommonly) used, and evidence-based treatment strategies determined not just by their referring surgeon but by current research.
This course investigates the latest surgical and minimally invasive techniques used and the benefits and risks associated with these techniques. Taking hundreds of nationally established joint protocols, presenter Trent Brown summarizes the most effective and functionally relevant treatment strategies and protocols. Numerous labs will occur to ensure application of material and immediate carry-over to the clinical setting. Mr. Brown will also discuss documentation techniques and examples to strongly justify the need for skilled services with this population in hospital, in-patient, acute, home health, and outpatient settings.
This is an intermediate level course.
Course Dates & Locations
Apr 25, 2026 – Apr 26, 2026
6100 Whipple Ave. NW, NORTH CANTON, OH 44720
Aultman North Canton Medical Center
6100 Whipple Ave. NW, NORTH CANTON, OH 44720
Educational Credit
A certificate of attendance for 15 Contact Hours will be awarded to each participant. All Therapy Network Seminars are pre‐approved for CEUs in the state where the course is conducted when required for PT, OT, ATs & Assistants.
Therapy Network, Inc. (BOC AP#: P2563) is approved by the Board of Certification, Inc. to provide continuing education to Certified Athletic Trainers. Our seminars are eligible for a maximum of 15 Category A hours/CEUs. ATs should claim only those hours actually spent in the educational program.
AOTA Approved Provider of Continuing Education # 3073 Category 1 Domain of OT. The assignment of AOTA CEUs does not imply endorsements of specific course content, products, or clinical procedures by AOTA
Audience
This is an intermediate level course intended for PTs, PTAs, OTs, OTAs and ATs
NOTE: Nothing in this course is to enable or permit the learner to apply techniques outside of the scope of practice in their individual state and discipline.
Objectives
- Identify the diagnostic, demographic, and lifestyle explanations related to an increase in joint arthroplasty and the increased need for therapy services following arthroplasty
- Identify and apply current evidence behind tissue healing science and how it affects the total joint client
- Identify the evidence justifying therapy following total joint arthroplasty and the long and short-term benefits of therapy
- Identify the difference between standard and reverse total arthroplasty components and techniques and how it impacts rehabilitation
- Demonstrate evidence based hip therapeutic strategies used for recovery of the most commonly used hip surgical techniques
- Identify the difference between the various surgical components and techniques used for knee arthroplasty and the impact of treatment
- Demonstrate the best treatment strategies for patients seen in any therapeutic setting following practice of techniques in lab
Schedule
-
Day 1
8:00 Registration and Continental Breakfast 8:30 Common Themes and Research behind Shoulder, Hip and Knee Arthroplasty (TSA, THA, TKA)
Demographics
Age, gender, lifestyle, and socioeconomic status
Inclusion criteria for TJA (based on AMA) and who should
avoid TJA
Common diagnosis, pain levels, and reduced functional
levels
Neurological and psychological consequences from delaying
total joint arthroplasty
Depression, sleep disturbances, confusion, and memory
loss
Healing stages
Inflammatory, proliferative, remodeling (over icing?)
Bone, cartilage, muscle, tendon, and nervous tissue
Review of joint movement and osteokinematics
Rolling, gliding, scapulohumeral rhythm, and spinning10:30 BREAK 10:45 Gait (Functional Mobility) and Arthroplasty The Determinants of Gait vs. Phases
-Minimizing COM Displacement pre-post arthroplasty
-Curtate-Prolate-COM Cycloid theories
-What the phases of gait neglect and how to address
following arthroplasty
-Why clients don’t fall performing “gait”
-How Shoulder, Hip, and Knee arthroplasty all impact
gait (pre and post-surgery)
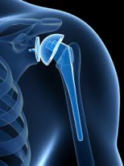
11:30 Total Shoulder Arthroplasty History leading to current procedures and prosthetics
-Functional verses textbook ROM for “normal” function
Procedures/components
-Glenoid component, humeral component
-Hemiarthroplasty, cemented vs. cementless, constrained
vs. non-constrained)
Reverse TSA
Why reverse TSA?
Minimally invasive R TSA including subscapularis sparing
12:00 LUNCH (ON YOUR OWN) 1:00 General therapeutic guidelines (3 or 4 phase approach)
-Goals, Precautions, Advancement Criteria (function vs.
a timeline)1:30 LAB: TSA Treatment
Phase 1:
-The proper pendulum
-Isometrics and elbow mechanics
Phase 2:
-4 approaches to GPG mobilization technique
-Non-WB scapular depression
-Natural arm swing and gait (standing/seated swingers)
3:00 BREAK 3:15 Phase 3 and 4
Functional carry-over
TSA failure rates, functional outcomes, and ROM
Appropriate “Functional” Standardized Assessments
4:00 Total Hip Arthroplasty History leading to current procedures and prosthetics
Normal versus functional ROM
Procedures/components
-Femoral component (cemented versus cementless)
-Acetabular component (plastic, metal, or ceramic)
-Anterolateral, posterolateral, direct lateral, anterior, and
superpath approaches
Advantages and disadvantages to each approach
5:30 Adjourn -
Day 2
8:00 LAB: General therapeutic guidelines Treatment
Phase 1 – 4 (Goals, Precautions, Advancement Criteria
(function vs. timeline)
Supine lateral stability (bed mobility)
Trochanter Tension
-Glut Med emphasis (what works? Evidence-based)
-Hip Hitch – Standing Sliders
-Pelvic Teeter Totter
10:00 BREAK 10:15 LAB: -Hip Flexor lengthening
-Lateral pelvic tilt in sitting leading to frontal plane
control (bed mobility)
-Seated Rotation
-Lateral weight shift - pelvic tilt emphasis (single leg
stance with resistance)
-Static Chops
Clinical Evidence behind THA and appropriate activities 12:00 LUNCH (ON YOUR OWN) 1:00 Total Knee Arthroplasty History leading to current procedures and prosthetics
- “Normal” range versus functional range
Procedures/components
-Femoral component (cemented versus cementless)
-Tibial component (metal platform with plastic surface for
ROM and absorption)
-Patellar component (metal or plastic)
-Cruciate retaining, posterior stabilized design, fixed
bearing, mobile bearing, and gender specific,
unicompartmental option
-Incisions (parapatellar, midvastus, subvastus/quad
sparing)
-Computer Aided Orthopedic Surgery (CAOS) why isn’t
being utilized?
1:45 LAB: General therapeutic guidelines Treatment
-Phase 1 – 4 (Goals, Precautions, Advancement Criteria
(function vs. timeline)
-Quad sit-up (NDT approach) (WB and functional
emphasis)
-4 directional Patellar Joint Mob
-AP/PA Tibiofemoral Joint Mob
2:30 BREAK 2:45 LAB Gold standard of the stationary bicycle
Knee Flexion 8* at Midstance
Gastroclock and Soleuostretch
Dynamic PNF Mobile Chops
4:15 Clinical Evidence behind TKA 4:30 Documentation Documentation ideas “outside the box” for the total joint
client
-Long-term care, acute, HH, outpatient, and transitional
clients
-Case study implementing research and treatment ideas
5:00 Course Evaluation and Adjourn
Cancellation Policy
Registration fee less a $75 administrative charge is refundable if cancellation received 14 days prior to program date. No refunds will be given after that time. Therapy Network, Inc. reserves the right to cancel a seminar and will refund in full the registration fee only. TNI is NOT responsible for registrants nonrefundable airfare, accommodations or fees.
Participants Comments